mD
The winter holidays are often described as magical—glowing lights, family gatherings, celebrations, and traditions that fill the season with joy. But as Kamerlin (2024) reminds us, this time of year can also bring complicated emotions. For many people, the holidays are not cheerful—they’re overwhelming, exhausting, or even painful. If you’re struggling, you’re not alone. And nothing is “wrong” with you for feeling this way. Holidays come with a cultural script: smile, celebrate, feel grateful. Kamerlin (2024) highlights how this pressure can turn normal stress or sadness into something heavier. When everyone else seems joyful, people often hide their struggles—leading to isolation, shame, and emotional exhaustion. Even positive events can be overwhelming. Preparing, hosting, traveling, managing finances, or navigating family dynamics can stretch anyone past their capacity. For those already coping with anxiety, trauma, chronic stress, or mental health conditions, the intensity of the season can amplify symptoms. The holidays tend to spotlight who is missing. Empty chairs at the table. Memories tied to traditions. Even if time has passed, grief often resurfaces—quietly, powerfully, unexpectedly. While some families gather with warmth, others gather with tension. Old wounds, unresolved conflict, or strained relationships may surface, and coping with these emotions can be draining. Gift-giving expectations, travel costs, and holiday events add financial pressure. Stress around money can quickly spiral into feelings of failure or hopelessness, especially in a season built around giving. Kamerlin (2024) emphasizes an overlooked truth: many people enter the holidays feeling alone—physically, emotionally, or both. Social media only magnifies this, making everyone else’s life look picture-perfect. Sleep changes, irregular meals, altered schedules, travel, and overstimulation can destabilize mental health—especially for individuals with anxiety, depression, bipolar disorder, or OCD. Structure matters, and the holidays often remove it. The holidays don’t have to be perfect. They don’t have to be happy. And they don’t have to look like anyone else’s. If this season feels heavy, give yourself permission to: Take breaks Set boundaries Say “no” without guilt Ask for help Create new traditions that feel safe Let go of expectations that don’t serve you Your emotional experience is valid—even if it doesn’t match the holiday music or TV commercials. If the holiday season brings up sadness, anxiety, grief, or overwhelm, CareSync Psych is here to support you through it. Whether you need therapy, medication management, stress-reduction strategies, or a safe space to talk, you don’t have to face this season alone. Compassion, understanding, and healing are possible—even in the middle of winter.Why the Holidays Can Trigger Depression
1. The Pressure to Be Happy
2. Emotional Overload
3. Grief Feels Sharper This Time of Year
4. Family Conflict and Relationship Stress
5. Financial Strain
6. Loneliness in a Season of Togetherness
7. Disruption of Routines
You’re Allowed to Feel What You Feel
Support Is Available
Is It Depression—Or Are You Low on Vitamin D? What You Need to Know
Is It Depression—Or Are You Low on Vitamin D? What You Need to Know
When you’re feeling down, exhausted, or emotionally flat, it’s easy to assume it’s “just depression.” But your mood is deeply connected to your body—and sometimes, symptoms of depression overlap with nutrient deficiencies that are surprisingly common.
One of the most overlooked contributors is low vitamin D.
Research over the past decade has consistently shown a strong link between vitamin D deficiency and depressive symptoms, making it an important piece of the mental health puzzle.
Vitamin D and Depression: What the Research Shows
According to Milaneschi et al. (2014), and other large population studies,—found that individuals with depressive disorders often have significantly lower vitamin D levels. This association holds true across ages, genders, and geographic locations.
Vitamin D Plays a Biological Role in Mood Regulation
Vitamin D is not just a nutrient, it acts more like a hormone. According to Menon et al. (2020), vitamin D receptors are found in brain regions responsible for mood, emotional regulation, and cognitive functioning. When vitamin D levels drop, these brain systems may not work as effectively.
Vitamin D Can Influence Key Neurotransmitters
Vitamin D has been shown to affect:
-
Serotonin production
-
Dopamine regulation
-
Inflammation pathways
These are the same pathways involved in depression, suggesting that vitamin D deficiency can contribute to symptoms—or worsen an existing depressive disorder.
Why Low Vitamin D Can Make You Feel Depressed
Vitamin D deficiency can create both emotional and physical symptoms that look—and feel—like depression.
Emotional/Mood Symptoms
-
Low mood
-
Irritability
-
Increased anxiety
-
Lack of motivation
-
Feeling “blah” or emotionally numb
Physical Symptoms That Can Be Misinterpreted as Depression
-
Fatigue
-
Muscle aches
-
Brain fog
-
Low energy
-
Sleep disturbances
-
Slow recovery from illness
When these physical symptoms happen alongside emotional ones, it’s natural to assume the cause is purely psychological. But sometimes the body is signaling a deeper imbalance.
Who Is Most at Risk of Vitamin D Deficiency?
You may be more vulnerable if you:
-
Spend most of your time indoors
-
Wear sunscreen or protective clothing often
-
Live in northern or low-sunlight areas
-
Have darker skin tones
-
Are overweight
-
Are pregnant or postpartum
-
Have autoimmune conditions
-
Experience chronic pain or inflammation
Understanding your risk can help you take proactive steps toward better health.
Why You Should Consider Checking Your Vitamin D Levels
If you’re experiencing depressive symptoms—or if your mood seems to change with the seasons—testing your vitamin D levels can give you valuable information.
It’s a simple blood test, and it may reveal a deficiency that’s contributing to how you feel. While vitamin D is not a replacement for therapy or medication, restoring normal levels may:
-
Improve mood stability
-
Reduce fatigue
-
Support better sleep
-
Decrease inflammation
-
Enhance overall mental well-being
Think of it as one more tool in a holistic, whole-body approach to mental health.
Talk with your provider about your vitamin D levels, and ask if your levels need to be checked.
CareSync Psych Can Help You Understand the Full Picture
At CareSync Psych, we look beyond symptoms—we look at you as a whole person. If you’re struggling with low mood, exhaustion, or emotional changes, we can help you determine whether vitamin D deficiency might be part of the issue.
Our team can:
-
Order vitamin D testing
-
Interpret your results
-
Create a tailored plan that may include supplementation, therapy, lifestyle changes, or medication management
When your mind and body work together, healing becomes more powerful.
Are You Struggling To Find Things To Be Grateful For In These Times?
IF GRATITUDE FEELS HARD RIGHT NOW…YOU ARE NOT ALONE
In a world filled with uncertainty, pressure, and constant change, it’s completely human to struggle with gratitude. Many people feel it—even if they don’t say it out loud.
But struggling with gratitude doesn’t mean anything is wrong with you.
It simply means you’re carrying a lot.
So instead of forcing yourself to find a silver lining, try this gentler truth:
💚 **Sometimes the bravest thing you can do is just keep going.**
💚 **Sometimes surviving *is* the victory.**
💚 **Sometimes gratitude begins with acknowledging how hard it’s been.**
These times are heavy. The world feels unpredictable. Many of us are simply trying to make it through the day, doing our best to survive emotionally, mentally, and physically. Gratitude can feel distant when life feels overwhelming.
You don’t need to have a long gratitude list. You don’t need to feel joyful. You don’t even need to have it all figured out. If you’re struggling to think of things to be grateful for, start with this simple truth:
✨ Be thankful for the chance to start over.
✨ Be thankful for the opportunity to change—even if it’s just a shift in mindset.
✨ Be thankful that growth doesn’t require perfection… only willingness.
At CareSync Psych, we want you to know that your feelings make sense. You don’t have to pretend. You don’t have to be endlessly positive. You don’t have to navigate this alone.
If today feels heavy… we’re here with you.
If the world feels uncertain… we understand.
And if you’re struggling to feel grateful… that’s okay.
Just keep showing up.
Keep breathing.
Keep going.
You matter—even on the days that feel hard. 💚
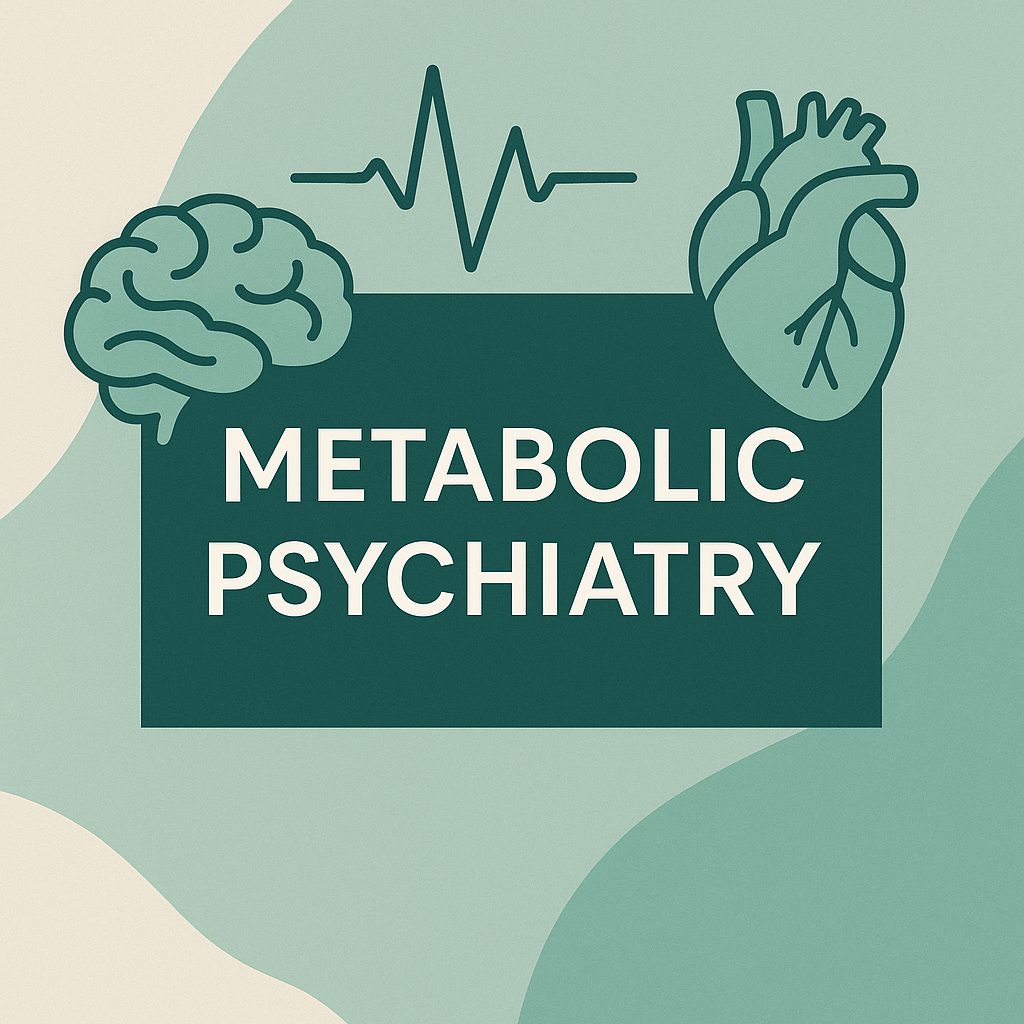
Metabolic Psychiatry
Metabolic Psychiatry is an emerging approach that focuses on how your health and metabolism impact your brain.
(And how it matters for mental health and overall wellness)
What do we mean by “glucose metabolism disorders”?
At its simplest: glucose metabolism refers to how your body handles sugar (glucose) — absorbing, using, storing, and regulating it. A “disorder” of glucose metabolism implies that one or more steps in that process is impaired, such that blood sugar levels run too high (hyperglycemia) or variably swing.
Common clinical entities include:
-
- Insulin resistance — when cells (muscle, fat, liver) become less responsive to insulin, so more insulin is needed to keep blood sugar in check. Wikipedia+1
- Prediabetes / impaired glucose tolerance — early dysregulation before full-blown type 2 diabetes
- Type 2 diabetes mellitus — sustained hyperglycemia because the system (insulin secretion + insulin sensitivity) fails to compensate adequately
- Hyperglycemia / elevated postprandial glucose — spikes of blood sugar after meals that stress the system Wikipedia+1
These metabolic disturbances are not just “lab numbers” — they interact deeply with inflammation, cell signaling, and systemic health, and may even influence cancer risk. Piątkiewicz & Czech (2011) review how altered glucose metabolism is implicated in cancer risk through pathways like oxidative stress, chronic inflammation, and dysregulation in cell proliferation. PubMed+2ResearchGate+2
Why is inflammation involved?
Inflammation and glucose dysregulation are tightly linked — each can exacerbate the other in a vicious cycle.
-
- In states of insulin resistance or hyperglycemia, there is increased oxidative stress and production of reactive oxygen species, which can trigger inflammatory pathways. Wiley Online Library+2PMC+2
- Pro-inflammatory cytokines (e.g. TNF-α, IL-6) impair insulin signaling and contribute to further insulin resistance. PMC+2AHADigital+2
- Metabolic inflammation (sometimes called “meta-inflammation”) is a low-grade, chronic inflammatory state associated with obesity, excess fat in tissues, dysregulated adipokines, and immune cell infiltration into metabolic organs (liver, fat, muscle). AHADigital+2JA Clinical Online+2
- In the Piątkiewicz & Czech framework, chronic dysregulation of glucose and insulin may also impair anti-cancer surveillance (for instance via effects on NK cells) and promote the microenvironment favoring tumorigenesis. Spandidos Publications+3PubMed+3ResearchGate+3
In short: when glucose metabolism is out of balance, it tends to fuel inflammation. In turn, that inflammation worsens metabolic regulation. Breaking the cycle is a key therapeutic goal.
Mental health, inflammation, and glucose metabolism
Because CareSync Psych is focused on psychiatric/psychological well-being, it’s worth noting:
-
- Inflammation is implicated in mood disorders, cognitive dysregulation, and neuropsychiatric conditions.
- Insulin resistance and hyperglycemia can influence brain energy metabolism, neuroinflammation, and neurotransmitter systems.
- Many psychotropic medications (e.g. some antipsychotics, mood stabilizers) have metabolic side effects — weight gain, insulin resistance — which increase vulnerability to glucose dysregulation and inflammation.
Thus, supporting better glucose homeostasis can have synergy with psychiatric care, improving not just physical health but potentially mental health outcomes.
What does the science say about Metabolic Psychiatry ?
Evidence-Based Strategies to Reduce Inflammation & Support Healthy Glucose Metabolism
Below are examples of possible strategies:
1. Dietary / Nutritional Modulation
-
- Emphasize whole, minimally processed foods: lots of vegetables, legumes, whole grains, lean proteins, nuts. This helps supply fiber, phytonutrients, antioxidants. PMC+3JA Clinical Online+3JACC+3
- Choose low-glycemic index/load carbohydrates to avoid huge post-meal glucose spikes. JACC+1
- Include anti-oxidant and anti-inflammatory nutrients — e.g. polyphenols, flavonoids, vitamins (C, E), carotenoids. The LWW article you referenced deals with how antioxidants may help buffer oxidative stress in the context of glucose disorders. Lippincott Journals
- Prioritize omega-3 fatty acids (from fatty fish, flax, chia) — these can help counter pro-inflammatory lipid signaling.
- Avoid or reduce ultraprocessed foods, added sugars, refined carbs — these contribute to inflammation, insulin spikes, and lipotoxicity. JA Clinical Online+2Wiley Online Library+2
- Consider “nutritional timing” / meal sequencing: Some research suggests that eating protein and fiber before carbs, or spreading carbs across the day, may blunt postprandial glycemic responses. JACC+1
- Modulate the gut microbiome: Dietary fiber (prebiotics), fermented foods, and supporting microbial diversity help maintain gut barrier integrity and reduce systemic endotoxin-driven inflammation. Wikipedia+1
2. Physical Activity & Exercise
-
- Exercise improves insulin sensitivity (especially in muscle) and helps glucose uptake independent of insulin.
- It also stimulates AMP-activated protein kinase (AMPK), a cellular “energy sensor” that helps shift metabolism toward more efficient, healthier processing. JA Clinical Online+3arXiv+3Nature+3
- Both aerobic and resistance training are beneficial; consistency is more important than intensity for most clients.
- Even moderate daily movement (e.g. walking after meals) can moderate postprandial glucose spikes and reduce inflammation.
3. Weight Management & Body Composition
-
- Excess adiposity (especially visceral fat) is strongly pro-inflammatory and contributes to insulin resistance.
- Gradual, sustainable weight loss can reduce inflammation, improve insulin sensitivity, and relieve metabolic stress. AHADigital+2PMC+2
4. Sleep, Circadian Rhythm & Stress Regulation
-
- Poor or insufficient sleep is associated with worse insulin sensitivity, dysregulated appetite hormones, and elevated inflammatory markers.
- Aligning eating/fasting windows with circadian rhythms (for example, avoiding late-night eating) may help glycemic control.
- Stress (psychological or physiological) raises cortisol, which antagonizes insulin and can push glucose higher — meditation, biofeedback, breathwork, psychotherapy are all relevant.
5. Pharmacological / Medical Adjuncts (in collaboration with providers)
-
- Some glucose-lowering medications also have anti-inflammatory effects. For example, metformin is believed to act beyond glucose, modulating inflammation via AMPK pathways. Wikipedia+2Nature+2
- Newer agents (e.g. semaglutide) are being studied for both metabolic and anti-inflammatory benefits. ScienceDirect
- In diabetes, certain drugs (e.g. thiazolidinediones) may reduce inflammation more than others for the same glycemic reduction. PMC+1
- Some studies are exploring immunometabolism (targeting metabolic pathways in immune cells) as a future anti-inflammatory strategy. Nature
6. Antioxidant Support & Supplementation (with caution)
-
- Because oxidative stress is a mediator between hyperglycemia and inflammation, antioxidants (dietary or supplemental) may help buffer the damage.
- But: indiscriminate high-dose antioxidant supplementation can have drawbacks (e.g. interfering with beneficial reactive oxygen signaling).
- It’s safer to prioritize obtaining antioxidants via whole foods (berries, dark greens, nuts, colorful vegetables) rather than “megadoses” of supplements.
- Book an Appointment
Metabolic Psychiatry involves how you eat, sleep, move, manage stress, and control blood sugar all change how your brain functions.
So instead of focusing only on symptoms like anxiety or depression, metabolic psychiatry also explores things like:
-
inflammation
-
insulin resistance
-
nutrient deficiencies
-
symptoms
-
chronic stress hormones
-
sleep and circadian rhythm
The goal is to treat mental health from both sides:
brain chemistry + whole-body biology.
Metabolic Psychiatry in Lakeland, Florida. In-person or telehealth available for the whole state of Florida.
References
Azzi, A., Davies, K. J., & Kelly, F. (2004). Free radical biology—Terminology and critical thinking. FEBS Letters, 558(1–3), 3–6.
Bastard, J. P., Maachi, M., Lagathu, C., Kim, M. J., Caron, M., Vidal, H., Capeau, J., & Feve, B. (2006). Recent advances in the relationship between obesity, inflammation, and insulin resistance. European Cytokine Network, 17(1), 4–12.
Czech, A., & Piątkiewicz, P. (2011). Glucose metabolism disorders and the risk of cancer. Archivum Immunologiae et Therapiae Experimentalis, 59(3), 215–230.
Dandona, P., Aljada, A., & Bandyopadhyay, A. (2004). Inflammation: The link between insulin resistance, obesity, and diabetes. Trends in Immunology, 25(1), 4–7. https://doi.org/10.1016/j.it.2003.10.013
Evans, J. L., Goldfine, I. D., Maddux, B. A., & Grodsky, G. M. (2002). Oxidative stress and stress-activated signaling pathways: A unifying hypothesis of type 2 diabetes. Endocrine Reviews, 23(5), 599–622. https://doi.org/10.1210/er.2001-0039
Giugliano, D., Ceriello, A., & Esposito, K. (2006). The effects of diet on inflammation: Emphasis on the metabolic syndrome. Journal of the American College of Cardiology, 48(4), 677–685. https://doi.org/10.1016/j.jacc.2006.03.052
Grundy, S. M. (2016). Metabolic syndrome update. Trends in Cardiovascular Medicine, 26(4), 364–373. https://doi.org/10.1016/j.tcm.2015.10.004
Hawley, J. A., & Lessard, S. J. (2008). Exercise training-induced improvements in insulin action. Acta Physiologica, 192(1), 127–135. https://doi.org/10.1111/j.1748-1716.2007.01783.x
Hotamisligil, G. S. (2017). Inflammation, metaflammation, and immunometabolic disorders. Nature, 542(7640), 177–185. https://doi.org/10.1038/nature21363
Piątkiewicz, P., & Czech, A. (2010). Antioxidants and glucose metabolism disorders. Current Opinion in Clinical Nutrition & Metabolic Care, 13(4), 512–518.
Rains, J. L., & Jain, S. K. (2011). Oxidative stress, insulin signaling, and diabetes. Free Radical Biology & Medicine, 50(5), 567–575. https://doi.org/10.1016/j.freeradbiomed.2010.12.006
Reaven, G. M. (2005). The insulin resistance syndrome: Definition and dietary approaches to treatment. Annual Review of Nutrition, 25(1), 391–406. https://doi.org/10.1146/annurev.nutr.24.012003.132155
Vozarova, B., Weyer, C., Hanson, K., Tataranni, P. A., Bogardus, C., & Pratley, R. E. (2001). Circulating interleukin-6 in relation to adiposity, insulin action, and insulin secretion. Obesity Research, 9(7), 414–417. https://doi.org/10.1038/oby.2001.54
Xu, H., Barnes, G. T., Yang, Q., Tan, G., Yang, D., Chou, C. J., … & Chen, H. (2003). Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. Journal of Clinical Investigation, 112(12), 1821–1830. https://doi.org/10.1172/JCI19451
Glucose and Hypometabolism
Cerebral glucose hypometabolism refers to a reduction in the brain’s ability to metabolize glucose, the primary source of neuronal energy. Because neurons have limited capacity for energy storage, consistent glucose supply is essential for proper cognitive, emotional, and behavioral function. When metabolism slows, neurons become less active, leading to impaired neurotransmission, synaptic plasticity, and overall brain performance — even before structural damage occurs.
🔬 Pathophysiology
Glucose metabolism in the brain occurs primarily through aerobic glycolysis, producing ATP to fuel neuronal signaling. When this process falters — whether due to mitochondrial dysfunction, neuroinflammation, insulin resistance, or oxidative stress — regions of the brain exhibit hypometabolism on FDG-PET (fluorodeoxyglucose positron emission tomography) scans.
Mechanisms contributing to cerebral hypometabolism include:
- Mitochondrial dysfunction: decreased ATP synthesis impairs neuronal signaling.
- Neuroinflammation: cytokines disrupt insulin and glucose pathways.
- Brain insulin resistance: glucose uptake is blunted despite normal peripheral insulin levels.
- Oxidative stress: damages neuronal membranes and enzymes critical for metabolism.
🧩 Clinical Correlations
Cerebral glucose hypometabolism is observed across neuropsychiatric and neurodegenerative disorders, with distinct regional patterns:
| Condition | Commonly Affected Regions | Clinical Correlates |
|---|---|---|
| Alzheimer’s Disease | Posterior cingulate, parietotemporal cortex | Early memory loss and executive dysfunction |
| Frontotemporal Dementia | Frontal and anterior temporal lobes | Behavioral disinhibition, apathy |
| Major Depressive Disorder | Dorsolateral prefrontal cortex, anterior cingulate | Impaired concentration, emotional regulation |
| Schizophrenia | Frontal and temporal regions | Executive dysfunction, cognitive impairment |
| Bipolar Disorder | Frontal, limbic circuits | Mood instability, impulsivity |
| Traumatic Brain Injury | Site-specific | Cognitive slowing, emotional dysregulation |
In psychiatry, hypometabolism often reflects neural circuit inefficiency rather than cell loss. For instance, decreased glucose utilization in the prefrontal cortex may explain poor emotional regulation in depression or executive dysfunction in schizophrenia.
⚕️ Integrative and Metabolic Psychiatry Perspective
At CareSync Psych, cerebral glucose hypometabolism underscores the mind-body connection — illustrating how metabolic and psychiatric processes intertwine. Emerging research links metabolic dysfunction (e.g., insulin resistance, obesity, chronic inflammation) with neuropsychiatric symptoms, suggesting that improving systemic metabolism may also enhance brain energy and mood stability.
Therapeutic approaches that can help restore cerebral metabolism include:
- Lifestyle interventions: balanced nutrition, exercise, restorative sleep.
- Nutritional psychiatry: ketogenic or low-glycemic diets supplying ketones as alternate brain fuel.
- Pharmacologic supports: metformin, GLP-1 receptor agonists, and mitochondrial antioxidants (e.g., CoQ10).
- Psychotherapy and mindfulness: reducing stress-driven cortisol spikes that impair glucose utilization.
🌿 Clinical Implications and Future Directions
- FDG-PET imaging remains the gold standard to detect regional hypometabolism.
- Metabolic psychiatry is reframing depression, anxiety, and cognitive decline as partly bioenergetic disorders.
- Addressing glucose dysregulation early may prevent progression of cognitive and emotional disorders.
- Future research aims to integrate metabolic biomarkers into psychiatric diagnostics and personalized treatment plans.
🧾 References (APA 7th Edition)
- Butterfield, D. A., & Halliwell, B. (2019). Oxidative stress, dysfunctional glucose metabolism, and Alzheimer disease. Nature Reviews Neuroscience, 20(3), 148–160. https://doi.org/10.1038/s41583-019-0132-6
- Cunnane, S. C., Trushina, E., Morland, C., Prigione, A., Casadesus, G., Andrews, Z. B., … & Mattson, M. P. (2020). Brain energy rescue: An emerging therapeutic concept for neurodegenerative disorders of ageing. Nature Reviews Drug Discovery, 19(9), 609–633. https://doi.org/10.1038/s41573-020-0072-x
- Mosconi, L., Berti, V., Glodzik, L., Pupi, A., De Santi, S., & de Leon, M. J. (2010). Pre-clinical detection of Alzheimer’s disease using FDG-PET, with or without amyloid imaging. Journal of Alzheimer’s Disease, 20(3), 843–854. https://doi.org/10.3233/JAD-2010-091504
- Rasgon, N. L., & McEwen, B. S. (2016). Insulin resistance—a missing link no more. Molecular Psychiatry, 21(12), 1648–1652. https://doi.org/10.1038/mp.2016.163
- Tomasi, D., & Volkow, N. D. (2019). Associations between brain activation, glucose metabolism, and psychiatric symptoms in major depressive disorder. Molecular Psychiatry, 24(12), 1672–1680. https://doi.org/10.1038/s41380-018-0262-9
- Zhang, X., Chen, W., Li, J., Zhang, Y., & Xu, Y. (2021). Brain glucose hypometabolism and psychiatric disorders: A review of mechanisms and therapeutic perspectives. Frontiers in Psychiatry, 12, 700–714. https://doi.org/10.3389/fpsyt.2021.700714
Food Addiction Treatment in Lakeland, Florida. Both in- person or telehealth appointments available for the state of Florida.
Many people struggling with food addiction describe a painful cycle: intense cravings, loss of control, guilt, and a promise to “do better tomorrow.” Yet this cycle isn’t simply about willpower. Research now shows that for some individuals, food addiction is a valid neurobiological and psychological condition—one that deserves understanding and compassionate, evidence-based treatment.
At CareSync Psych, we help patients recognize that food addiction is not a moral failure—it’s a complex interaction between the brain, body, and emotional regulation systems.
Is Food Addiction Real?
The concept of “food addiction” has been debated for years. However, growing evidence supports that highly palatable foods—especially those rich in sugar, fat, and salt—can activate the same neural reward pathways as drugs of abuse.
-
- According to Gordon et al. (2018), a systematic review and found strong evidence linking addictive-like eating patterns to the dopamine-driven reward system seen in substance use disorders.
- Fletcher & Kenny (2018) concluded that food addiction shares behavioral, neurochemical, and genetic overlaps with traditional addictions.
- Davis (2013) also discussed that binge eating disorder (BED) and food addiction share common features such as loss of control, tolerance, and withdrawal symptoms.
In other words, the brain can become “hooked” on certain foods in much the same way it becomes hooked on drugs—especially ultra-processed foods that hijack our reward system.
The Brain–Body Mechanisms Behind Food Addiction
1. Dopamine Dysregulation in Food Addiction
When we eat hyperpalatable foods, the brain releases a surge of dopamine in the nucleus accumbens—the same reward area activated by drugs like cocaine or opioids. Over time, the brain may require more of that stimulus to achieve the same pleasure, leading to cravings and compulsive eating.
2. Stress and Cortisol‘
Chronic stress triggers cortisol, increasing appetite and preference for “comfort foods.” This stress-eating loop reinforces emotional dependency on food as a coping mechanism.
3. Insulin and Leptin Resistance
Biological changes in metabolism, especially insulin resistance, blunt hunger and satiety cues, making it harder to regulate intake. The body craves quick energy even when it doesn’t need it.
4. Gut–Brain Axis
Emerging evidence suggests gut microbiome imbalances can alter neurotransmitter production and cravings—linking digestion, emotion, and appetite regulation in a powerful feedback loop.
The Emotional and Mental Health Connection
Food addiction rarely exists in isolation. It’s often intertwined with anxiety, depression, trauma, and obsessive-compulsive tendencies.
-
- Many people use food for emotional regulation—to numb, soothe, or escape discomfort.
- Feelings of shame and guilt after overeating can trigger further stress, fueling another cycle of bingeing.
- Early life adversity and attachment disruptions may increase vulnerability by altering stress responses and reward sensitivity.
As Davis (2013) describes, these overlapping mechanisms mean that treating food addiction requires addressing both biological and psychological roots.
Why We Feel “Out of Control” & Why Food Addiction is Real
When people say, “I know I shouldn’t eat it, but I can’t stop myself,” they are describing the very essence of addiction—a disconnect between intention and behavior. This sense of loss of control comes from changes in the brain’s prefrontal cortex, the region responsible for decision-making and impulse control.
Repeated exposure to addictive foods dulls this region’s inhibitory capacity, while the limbic system (reward/emotion) becomes more dominant. The result: even when we consciously want to stop, our neurobiology keeps pushing us toward the next “fix.”
Healing Through Understanding and Integration
At CareSync Psych, we approach food addiction through the lens of metabolic psychiatry and compassionate behavioral therapy. Healing begins by syncing the mind and body.
Our approach includes:
-
- Psychotherapy and Mindfulness-Based Interventions to explore emotional triggers, perfectionism, and shame.
- Metabolic and Nutritional Assessment to stabilize blood sugar, reduce inflammation, and restore neurotransmitter balance.
- Medication-Assisted and Supplement Support (when indicated) targeting dopamine or serotonin pathways.
- Lifestyle and Behavioral Strategies including stress management, movement, and restorative sleep to reset the body’s reward systems.
Recovery isn’t about deprivation—it’s about reclaiming control, reconnecting with internal hunger and fullness cues, and healing the relationship with both food and self.
The Takeaway
Food addiction is not a weakness—it’s a neurobiological reality rooted in survival mechanisms that have been hijacked by modern food environments. Understanding it as both a mental health and metabolic issue allows for deeper compassion and more effective treatment.
At CareSync Psych, we believe recovery begins when you stop blaming yourself and start treating both your brain chemistry and emotional wounds together—because healing happens when mind and body finally sync.
📖 References
-
- Gordon, E. L., Ariel-Donges, A. H., Bauman, V., & Merlo, L. J. (2018). What is the evidence for “food addiction?” A systematic review. Nutrients, 10(4), 477. https://doi.org/10.3390/nu10040477
- Fletcher, P. C., & Kenny, P. J. (2018). Food addiction: a valid concept? Neuropsychopharmacology, 43(13), 2506–2513. https://doi.org/10.1038/s41386-018-0203-9
- Davis, C. (2013). Compulsive overeating as an addictive behavior: overlap between food addiction and binge eating disorder. Current Obesity Reports, 2(2), 171–178. https://doi.org/10.1007/s13679-013-0049-x
For decades, psychiatry has focused heavily on neurotransmitters—serotonin, dopamine, norepinephrine—as the “big three” of mental health. But new science is showing that the mind is not separate from the body. Instead, our mental health is tightly linked with our diet, metabolism, and even the way our mitochondria produce energy. This growing field—metabolic psychiatry—is reshaping how we understand and treat conditions like depression, anxiety, and other psychiatric disorders.
Book an Appointment
The Metabolic–Mental Health Connection
Research has uncovered a bidirectional relationship between depression and metabolic syndrome, a condition marked by obesity, high blood pressure, high cholesterol, and insulin resistance. In a groundbreaking Mendelian randomization study, Zhang et al. (2021) demonstrated that not only does metabolic syndrome increase the risk of depression, but depression itself may worsen metabolic health—creating a vicious cycle that traps patients in both poor physical and mental health.
This finding highlights an important truth: when we treat the body, we treat the brain, and when we treat the brain, we treat the body.
The Role of Mitochondria and Tryptophan Pathways
Our mental state depends on how well our brain cells produce and use energy. Mitochondrial impairment—the reduced ability of cells’ “powerhouses” to generate energy—has emerged as a common factor in psychiatric disorders. Tanaka et al. (2022) emphasize the link between dysfunctional mitochondria and disturbances in the tryptophan–kynurenine pathway, which regulates serotonin and neuroprotective metabolites. When this pathway is imbalanced, patients may experience both mood disorders and cognitive changes.
This suggests that psychiatric symptoms are not just “chemical imbalances” but may also reflect underlying metabolic and cellular dysfunction.
Diet as a Foundation for Mental Health
Dietary patterns directly influence brain health. Diets high in refined sugars and processed foods can promote inflammation, insulin resistance, and mitochondrial stress—all of which worsen depression and anxiety. Conversely, nutrient-dense diets rich in omega-3 fatty acids, antioxidants, fiber, and amino acids like tryptophan can support healthier brain signaling and energy metabolism.
Examples include:
-
Mediterranean-style diets, associated with reduced depression risk.
-
Ketogenic or low-carbohydrate approaches, which stabilize insulin and may improve treatment-resistant mood disorders.
-
Anti-inflammatory foods (leafy greens, fatty fish, berries), which reduce oxidative stress on the brain.
Revolutionary Treatment Approaches in Metabolic Psychiatry
What makes this field revolutionary is that it goes beyond traditional antidepressants by addressing root causes in metabolism. Innovative strategies include:
-
Metabolic Medications with Psychiatric Impact
-
Drugs like metformin (used for diabetes) are being studied for depression in insulin-resistant patients.
-
GLP-1 receptor agonists (like semaglutide) may also reduce both metabolic burden and depressive symptoms.
-
-
Targeting Mitochondria
-
Nutritional supplements such as CoQ10, NAD+ precursors, and certain amino acids may support mitochondrial resilience.
-
Therapies that restore mitochondrial function could improve both mood and cognition.
-
-
Diet-Based Interventions
-
Structured programs integrating dietary counseling into psychiatric care are being tested to break the depression–metabolic syndrome cycle.
-
-
Integrated Care Models
-
Combining psychiatric and metabolic treatments into holistic, whole-person care may offer the most promise. Patients with depression, obesity, and metabolic syndrome benefit most when both aspects are treated together rather than separately.
-
Book an Appointment
A New Horizon: Treating the Whole Person
The future of psychiatry lies in seeing mental health through the lens of metabolic health. Instead of separating “brain” and “body,” metabolic psychiatry brings them together, creating space for innovative therapies that restore balance at the cellular and systemic level.
By focusing on diet, metabolism, and mitochondrial health, we move toward revolutionary treatment approaches that sync the mind and body, ultimately offering hope for patients who haven’t found relief through traditional psychiatric care.