Why Insulin Resistance Matters—Even When Blood Sugar Is “Normal”
You might have insulin resistance even though your glucose levels are normal; this can impact your physical and mental health.
Many people are told their labs are “normal” and assume their metabolic health is fine—especially when fasting glucose falls within the expected range. Yet growing research shows that insulin sensitivity often declines years before blood sugar becomes abnormal. This hidden phase of metabolic dysfunction can quietly affect brain health, mood, energy, weight regulation, and inflammation, long before diabetes ever appears.
At CareSync Psych, we take a mind-body approach to mental health. Understanding insulin sensitivity is a critical part of that picture.
CareSync Psych in Lakeland Florida
-helps patients across Florida understand insulin resistance, metabolic health, and inflammation through metabolic psychiatry. Even with normal blood sugar, impaired insulin sensitivity may drive metabolic dysfunction, obesity, and prediabetes
Insulin Sensitivity vs. Blood Sugar: What’s the Difference?
Insulin Sensitivity vs. Blood Sugar: What’s the Difference?
Glucose is the sugar circulating in your bloodstream.
Insulin is the hormone that helps move glucose from the blood into cells so it can be used for energy.
-
Good insulin sensitivity = cells respond easily to insulin
-
Insulin resistance = cells stop responding well, so the body must release more insulin to keep blood sugar normal
Here’s the key point:
👉 Blood sugar can stay normal for years while insulin levels are chronically elevated.
This is why fasting glucose alone often misses early metabolic dysfunction.
You might have insulin resistance even though your glucose levels are normal; this can impact your physical and mental health.
Many people are told their labs are “normal” and assume their metabolic health is fine—especially when fasting glucose falls within the expected range. Yet growing research shows that insulin sensitivity often declines years before blood sugar becomes abnormal. This hidden phase of metabolic dysfunction can quietly affect brain health, mood, energy, weight regulation, and inflammation, long before diabetes ever appears.
At CareSync Psych, we take a mind-body approach to mental health. Understanding insulin sensitivity is a critical part of that picture.
CareSync Psych in Lakeland Florida helps patients across Florida understand insulin resistance, metabolic health, and inflammation through metabolic psychiatry. Even with normal blood sugar, impaired insulin sensitivity may drive metabolic dysfunction, obesity, and prediabetes (Radziuk, 2000; Schenk et al., 2008).
Insulin Sensitivity vs. Blood Sugar: What’s the Difference?
You might have insulin resistance even though your glucose levels are normal; this can impact your physical and mental health.
At CareSync Psych, we take a mind-body approach to mental health. Understanding insulin sensitivity is a critical part of that picture.
Glucose is the sugar circulating in your bloodstream.
Insulin is the hormone that helps move glucose from the blood into cells so it can be used for energy.
-
Good insulin sensitivity = cells respond easily to insulin
-
Insulin resistance = cells stop responding well, so the body must release more insulin to keep blood sugar normal
Here’s the key point:
👉 Blood sugar can stay normal for years while insulin levels are chronically elevated.
This is why fasting glucose alone often misses early metabolic dysfunction.
Why Insulin Resistance Is a Better Early Marker of Metabolic Health
Research consistently shows that insulin resistance develops first, while glucose abnormalities come later (Radziuk, 2000).
During this stage:
-
The pancreas compensates by producing more insulin
-
Blood sugar appears “normal” on routine labs
-
Inflammation and metabolic stress increase quietly
Why Insulin Resistance Is a Better Early Marker of Metabolic Health
Research consistently shows that insulin resistance develops first, while glucose abnormalities come later (Radziuk, 2000).
During this stage:
-
The pancreas compensates by producing more insulin
-
Blood sugar appears “normal” on routine labs
-
Inflammation and metabolic stress increase quietly
“Insulin-Sensitive Obesity” vs. “Hidden Insulin Resistance”
Interestingly, not all metabolic dysfunction looks the same.
Some individuals with higher body weight remain relatively insulin sensitive, while others—often at a “normal” weight—develop insulin resistance (Klöting et al., 2010). This means:
-
Weight alone does not define metabolic health
-
Thin individuals can still have significant insulin resistance
-
Mental health symptoms may appear before physical signs
This is especially relevant in psychiatry, where fatigue, depression, anxiety, brain fog, and poor stress tolerance may have metabolic contributors.
How Insulin Resistance Affects the Brain and Mental Health
Insulin plays a role far beyond blood sugar control. In the brain, insulin signaling supports:
-
Neurotransmitter balance
-
Cognitive function
-
Mood regulation
-
Stress response
When insulin resistance develops, chronic low-grade inflammation increases and brain signaling becomes less efficient (Schenk et al., 2008).
This inflammatory state has been linked to:
-
Depression
-
Anxiety
-
Cognitive slowing
-
Increased stress sensitivity
-
Difficulty regulating appetite and energy
This is one reason metabolic psychiatry looks upstream—before symptoms become entrenched.
Why “Normal Labs” Don’t Always Mean Optimal Health
Standard labs often focus on fasting glucose or A1C, which detect problems only after insulin resistance has progressed significantly. Earlier markers may include:
-
Elevated fasting insulin
-
HOMA-IR
-
Triglyceride-to-HDL ratio
-
Signs of systemic inflammation
By the time glucose rises, insulin resistance has often been present for years.
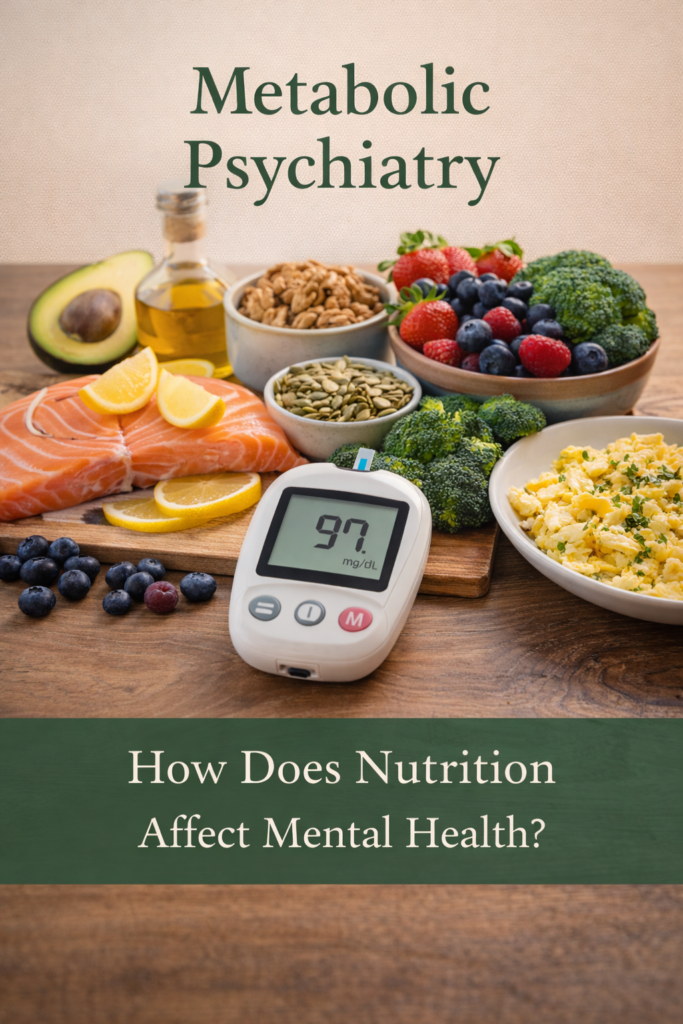
A Metabolic Psychiatry Perspective
At CareSync Psych, we believe mental health care works best when it addresses underlying physiology, not just symptoms. Measuring insulin sensitivity helps us:
-
Identify early metabolic stress
-
Personalize treatment plans
-
Support mood, cognition, and energy more effectively
-
Integrate lifestyle, nutrition, and medical strategies thoughtfully
This approach does not replace psychiatric care—it enhances it by treating the whole person.
CareSync Psych in Lakeland Florida helps patients across Florida understand insulin resistance, metabolic health, and inflammation through metabolic psychiatry.
Even with normal blood sugar, impaired insulin sensitivity may drive metabolic dysfunction, obesity, and prediabetes.
What should you keep in mind?
-
Insulin resistance often appears before blood sugar abnormalities
-
Normal glucose does not guarantee metabolic health
-
Insulin sensitivity is a more sensitive early marker of dysfunction
-
Metabolic health and mental health are deeply interconnected
By identifying these patterns early, we can support long-term mental and physical well-being—before disease develops.