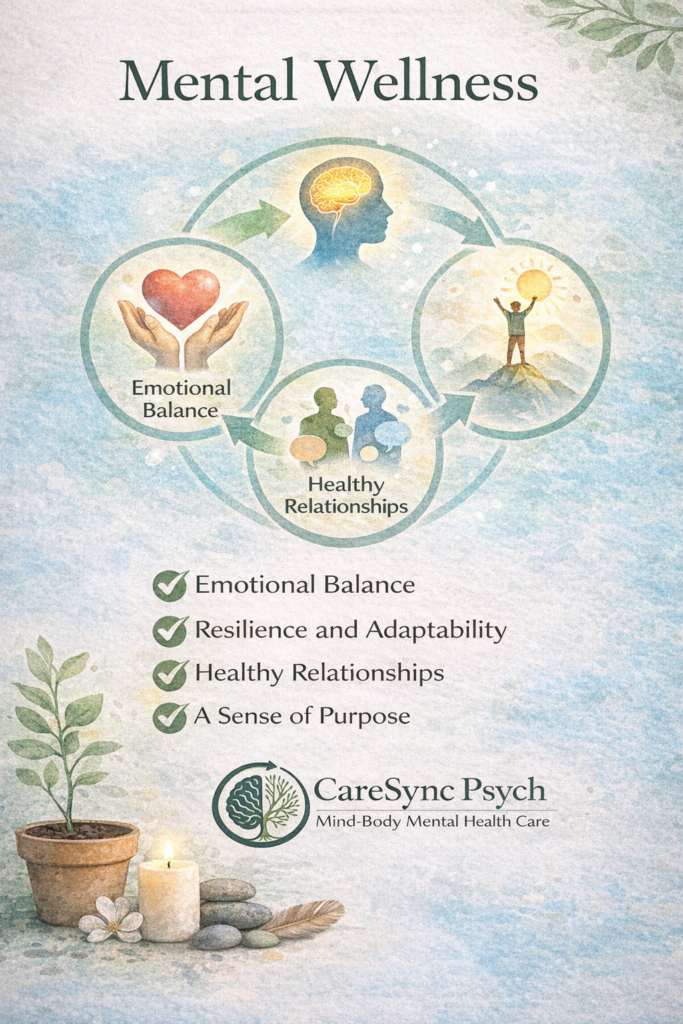
What Is Mental Wellness?
And How Do We Actually Achieve It?
Mental wellness is more than the absence of mental illness. It is a dynamic, evolving state of emotional balance, psychological resilience, social connection, and purpose.
At CareSync Psych, we view mental wellness as the ability to:
-
Regulate emotions effectively
-
Adapt to stress
-
Maintain meaningful relationships
-
Experience purpose and fulfillment
-
Function in daily life with clarity and stability
This definition aligns with contemporary psychiatric literature emphasizing that mental well-being is multidimensional and influenced by biological, psychological, and social factors (Gautam et al., 2024).
Mental Health vs. Mental Wellness
Mental health often refers to diagnosable conditions (e.g., anxiety disorders, depression, bipolar disorder).
Mental wellness refers to:
-
How well you are functioning
-
How resilient you feel
-
How connected and purposeful your life feels
Gautam et al. (2024) describe mental well-being as shaped by determinants such as:
-
Genetics and neurobiology
-
Life experiences and trauma
-
Socioeconomic context
-
Social support
-
Coping skills
In other words, mental wellness is not just internal—it is influenced by environment and lived experience.
What Impacts Mental Wellness?
Research consistently shows that stress is one of the strongest predictors of reduced mental well-being.
Slimmen et al. (2022) found that stressors and perceived stress significantly influence mental well-being, particularly when individuals lack effective coping strategies. Importantly, it is not only the presence of stress—but how we interpret and manage it—that determines outcomes.
Common stress-related disruptors of mental wellness include:
-
Chronic workload or academic pressure
-
Financial strain
-
Relationship conflict
-
Poor sleep
-
Social isolation
-
Unresolved trauma
When stress becomes chronic, it affects emotional regulation, immune function, sleep cycles, and cognitive clarity.
The Components of Mental Wellness
Cardozo et al. (2023) describe mental wellness as involving:
1. Emotional Regulation
The ability to identify and manage feelings without becoming overwhelmed.
2. Cognitive Flexibility
Being able to adapt to change and shift perspective.
3. Social Connectedness
Healthy relationships are protective factors for mental well-being.
4. Purpose and Meaning
A sense that one’s life has direction and value.
5. Self-Efficacy
Belief in one’s ability to handle challenges.
Mental wellness is therefore both internal (mindset, coping) and external (relationships, environment, lifestyle).
How Do We Accomplish Mental Wellness?
Mental wellness is not achieved through a single intervention. It is cultivated.
Here are evidence-informed ways to strengthen mental wellness:
1. Develop Adaptive Coping Skills
Healthy coping includes:
-
Problem-solving
-
Mindfulness practices
-
Cognitive reframing
-
Emotional expression
Maladaptive coping (avoidance, substance reliance, rumination) tends to reduce long-term wellness (Gautam et al., 2024).
2. Manage Stress Proactively
Stress reduction strategies may include:
-
Structured routines
-
Sleep regulation
-
Time boundaries
-
Therapy
-
Physical activity
Slimmen et al. (2022) emphasize that perceived stress mediates the relationship between life stressors and well-being—meaning our regulation strategies matter deeply.
3. Strengthen Social Support
Humans are relational. Social connection protects against anxiety and depressive symptoms. Even small improvements in connection can enhance mental wellness.
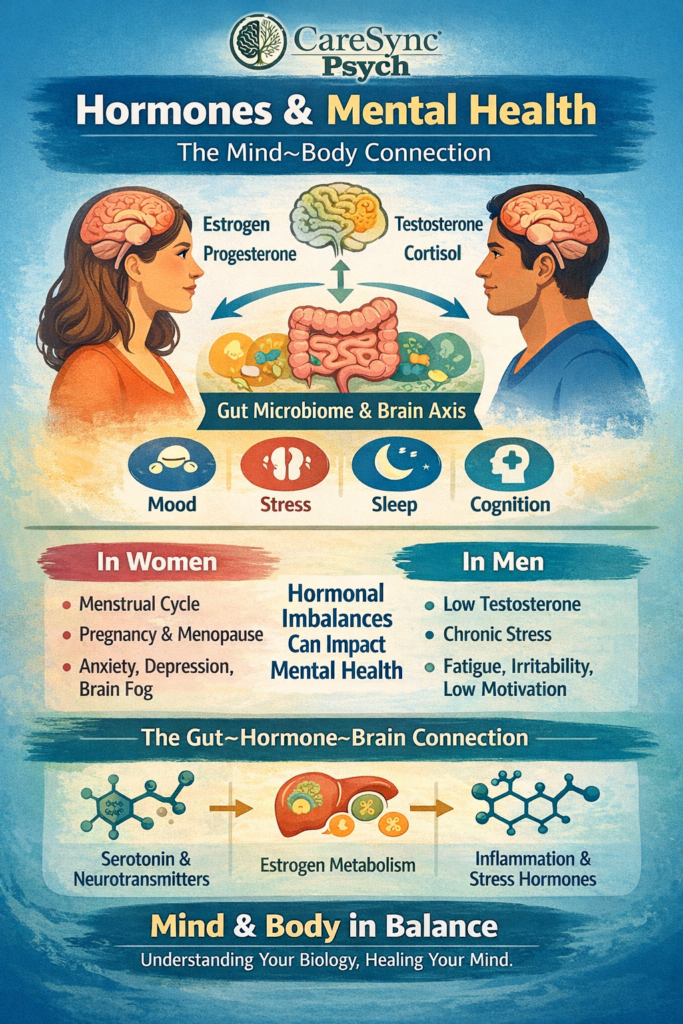
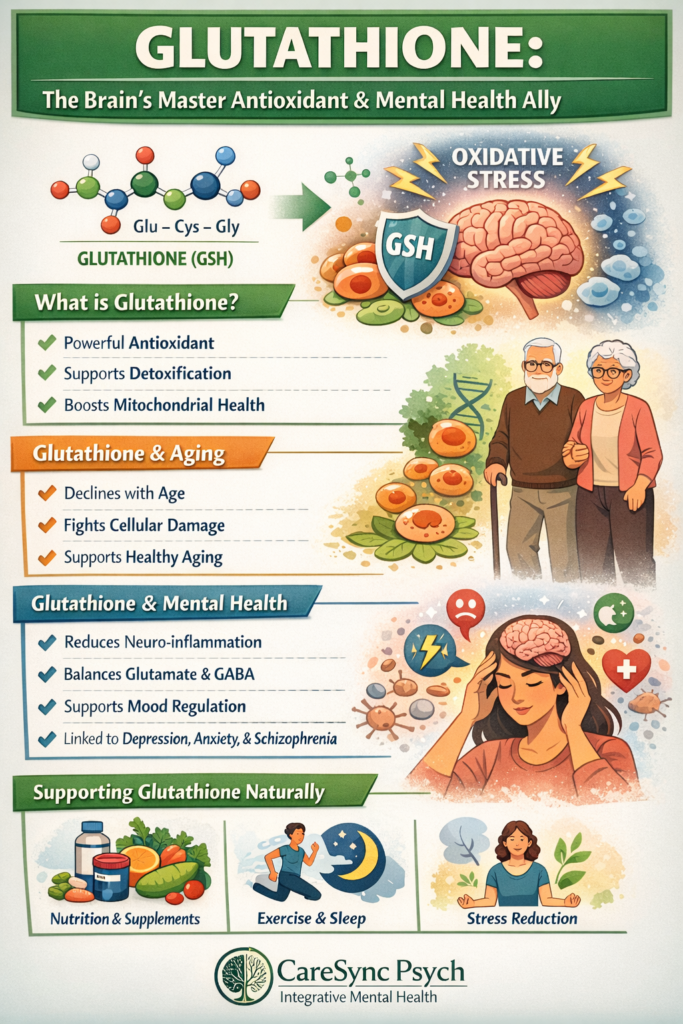
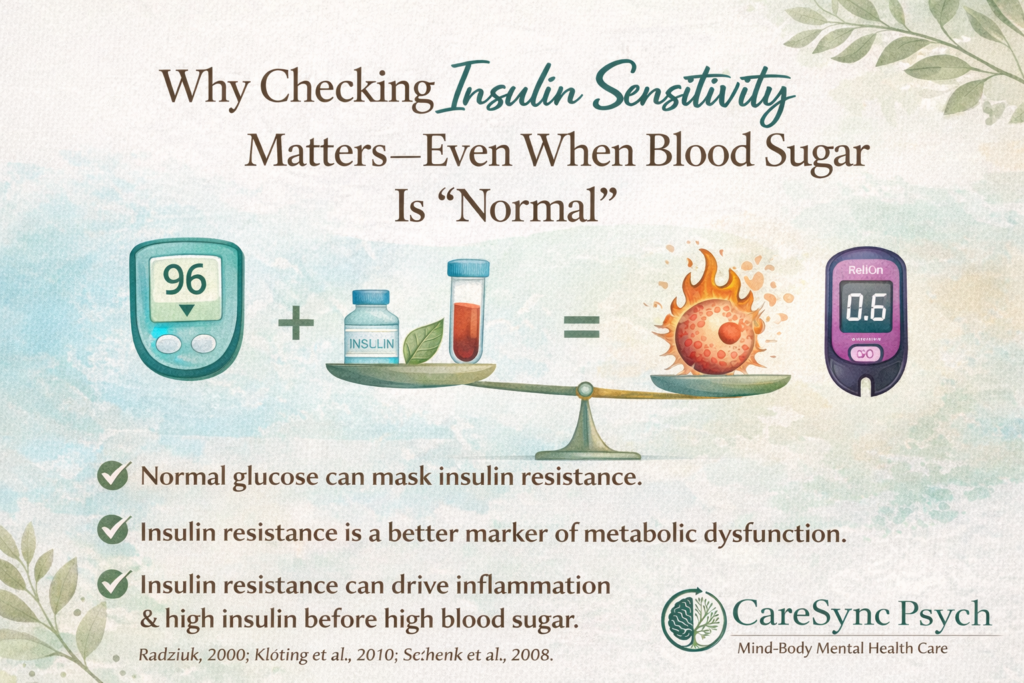
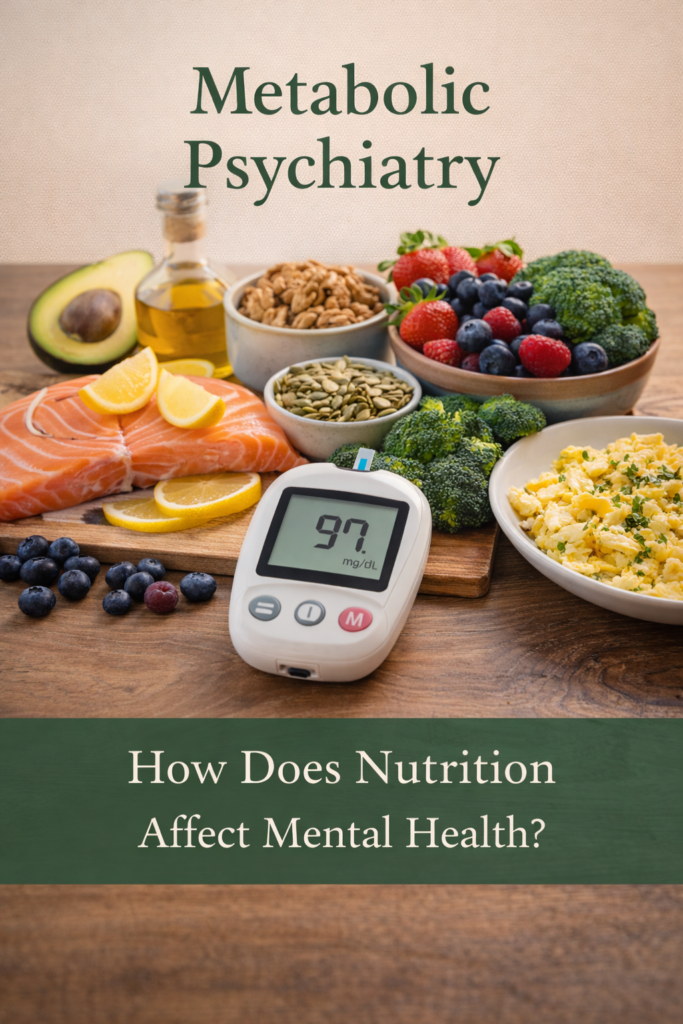
4. Align Lifestyle With Brain Health
Sleep, nutrition, movement, and metabolic health influence mood regulation, inflammation, and cognitive clarity.
Mental wellness is biological as much as psychological.
5. Seek Professional Support When Needed
Therapy and medication are not signs of weakness. They are tools for restoring balance when stress overwhelms coping capacity.
At CareSync Psych, we integrate:
-
Medication management (when appropriate)
-
Psychotherapy
-
Lifestyle interventions
-
Education and skill-building
Because wellness is comprehensive.
Mental Wellness Is Not Perfection
It does not mean:
-
Always feeling happy
-
Never experiencing stress
-
Being “productive” at all times
It means having the capacity to navigate difficulty without losing stability.
Wellness fluctuates. Resilience grows.
The CareSync Psych Perspective
Mental wellness is not something you either have or do not have—it is something you cultivate.
Through supportive care, structured coping strategies, metabolic awareness, and relational healing, mental wellness becomes attainable.
It is not about eliminating struggle.
It is about strengthening your ability to move through it.
.
References
Cardozo, F., Pahuja, V., Samvedi, D., Madat, O., & Bhatia, G. (2023). Mental wellness—Mind matters. In International Conference on Information and Communication Technology for Intelligent Systems (pp. 295–304). Springer Nature Singapore.
Gautam, S., Jain, A., Chaudhary, J., Gautam, M., Gaur, M., & Grover, S. (2024). Concept of mental health and mental well-being, its determinants and coping strategies. Indian Journal of Psychiatry, 66(Suppl 2), S231–S244.
Slimmen, S., Timmermans, O., Mikolajczak-Degrauwe, K., & Oenema, A. (2022). How stress-related factors affect mental wellbeing of university students: A cross-sectional study to explore the associations between stressors, perceived stress, and mental wellbeing. PLOS ONE, 17(11), e0275925.