What Is Metabolic Psychiatry?
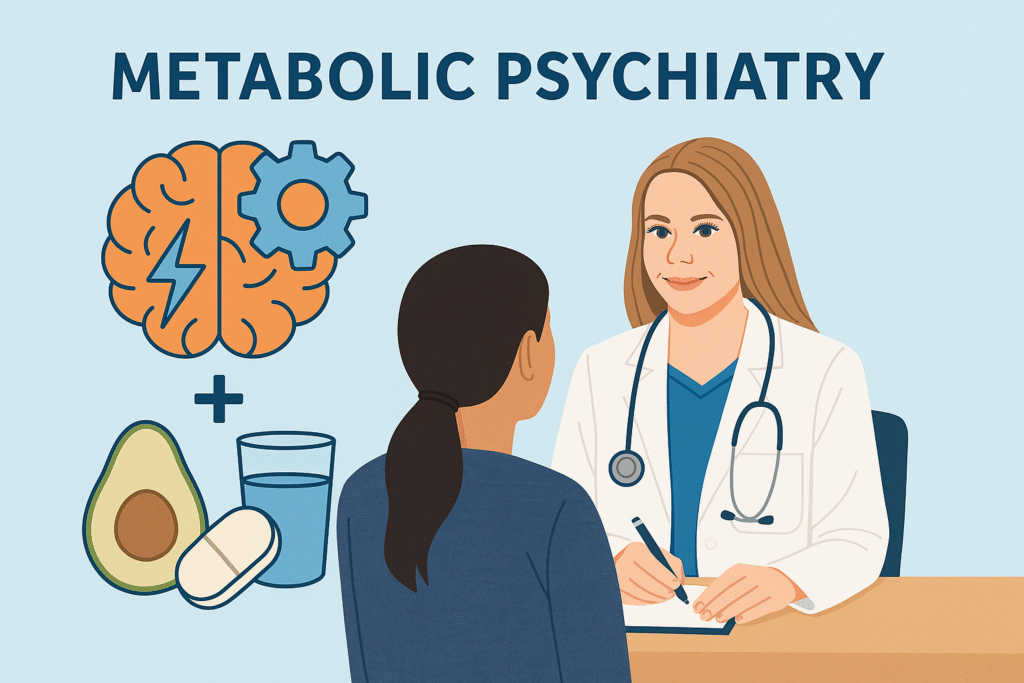
Metabolic psychiatry is an emerging approach that looks at how the health of your body—especially your metabolism—affects the health of your brain.
In simple terms:
🧠 Your brain is not separate from your body.
How you eat, sleep, move, manage stress, and control blood sugar all change how your brain functions.
So instead of focusing only on symptoms like anxiety or depression, metabolic psychiatry also explores things like:
The goal is to treat mental health from both sides:
brain chemistry + whole-body biology.
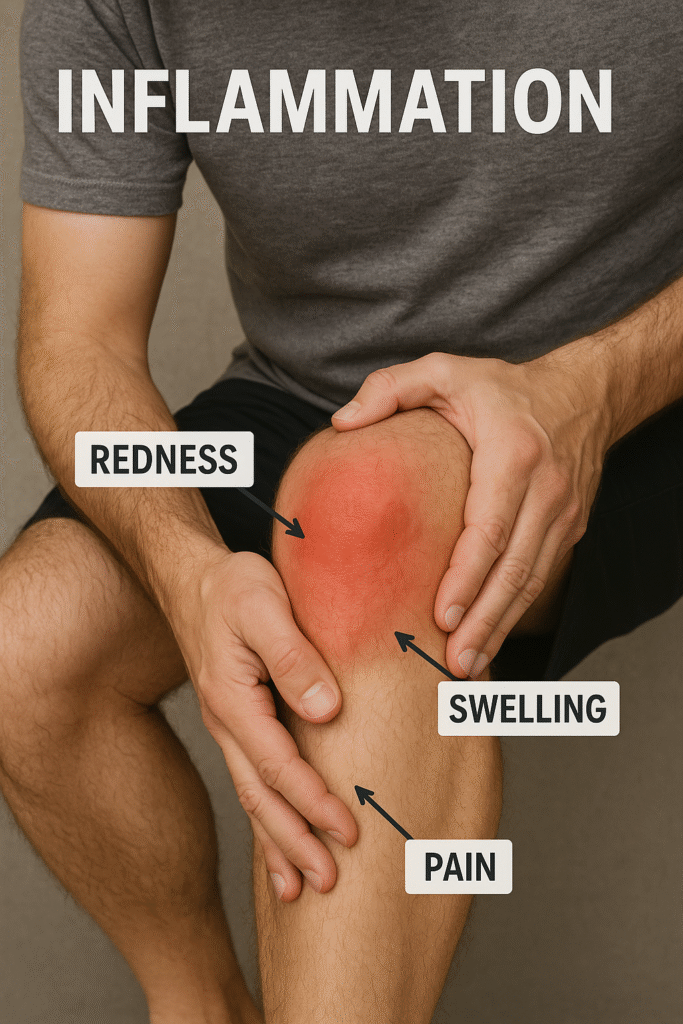
🔥 How Inflammation Affects Mental Health
Inflammation is your body’s alarm system.
When it’s short-term, it protects you.
But when it becomes chronic, it can quietly disrupt brain function.
Chronic inflammation can:
-
interfere with serotonin and dopamine
-
affect energy and fatigue
-
increase anxiety sensitivity
-
intensify pain perception
-
impair focus and memory
Think of it like this:
👉 A brain that is constantly “on fire” can’t regulate emotions well.
People with chronic inflammation often report:
-
feeling more irritable
-
fatigue or brain fog
-
low mood
-
poor motivation
-
sleep trouble
Inflammation can come from:
-
processed foods
-
sedentary lifestyle
-
disturbed sleep
-
long-term stress
-
obesity
-
autoimmune disease
-
infections
So, when providers evaluate mood—they should also look for biological contributors, not just psychological ones.